Prof. Dr. Laszlo Kovacs from the Department of Plastic Surgery and Hand Surgery (Klinikum rechts der Isar der Technischen Universität München) initiated the research group Computer Aided Plastic Surgery (CAPS).
The leading idea of this group is the fusion of various disciplines e.g. bioengineering, mathematics, physics, biomechanics, computer science and other associated disciplines in order to create new knowledge and solutions with benefit for interdisciplinary problems.
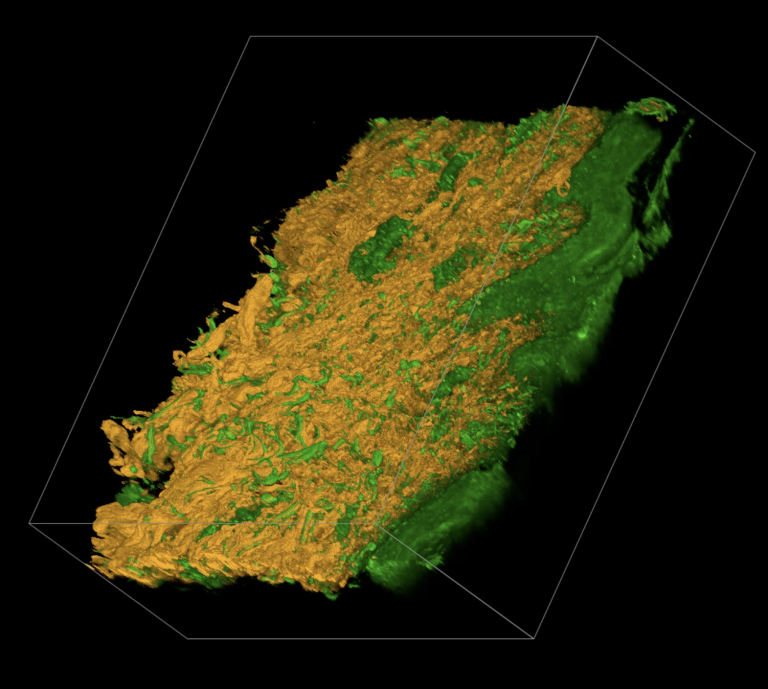
The scientific focus of CAPS evaluates innovative technologies for the 3-D assessment, digitalization and visualisation of the human body surface and soft tissues to implement computer aided surgery (CAS) into the field of aesthetic, plastic and reconstructive surgery.